Can you breastfeed with breast implants and is this safe for the breastfed baby? This article looks at whether breastfeeding with implants is possible, how breast implants affect milk supply and whether breastfeeding with implants is safe for the breastfed baby.
What are implants?
Breast implants are soft man-made silicone structures that are inserted under the skin to reshape and/or enlarge breasts.

Can you breastfeed with implants?
Although it is often possible to breastfeed with implants, they may affect a mother’s capacity to produce a full milk supply and there is very little research on long term health of babies born to, or breastfed from, mothers with breast implants. Whether a mother will have a full or only a partial milk supply depends on the type of breast surgery involved and the amount of damage to nerves or breast tissue. It will also depend on how much functional milk-making (glandular) tissue is present both before and after the procedure.
As with every breastfeeding experience, success also depends on having the right information about latch (the way baby attaches to the breast), positioning, making more milk and breastfeeding management.
all women who have had augmentation surgery face the possibility of compromising maximum milk volume not only from the site of the incision but also from nerve disruption and pressure from the implant on breast structures
How do breast implants affect breastfeeding?
Breast implants can reduce a mother’s milk supply. Breast function can be affected by;
#1 Location of the incision
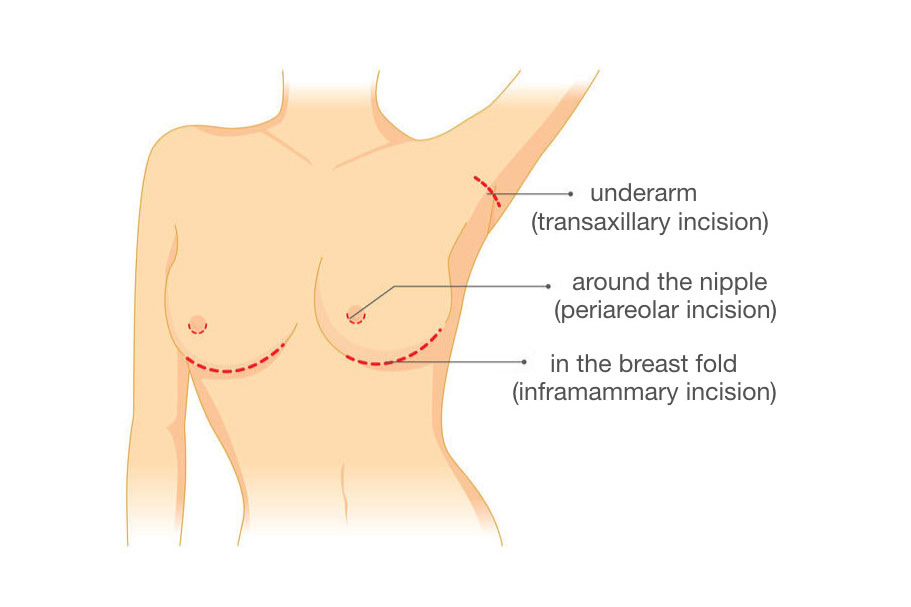
The position of the cut (incision) and the way an implant is inserted affect how much damage there is to nerves, milk glands, ducts or the blood supply in the breast. For example, an incision around the edge of the areola (the darker skin around the nipple) is more likely to damage the nerve that is critical to nipple sensitivity and the let-down reflex (release of breast milk).
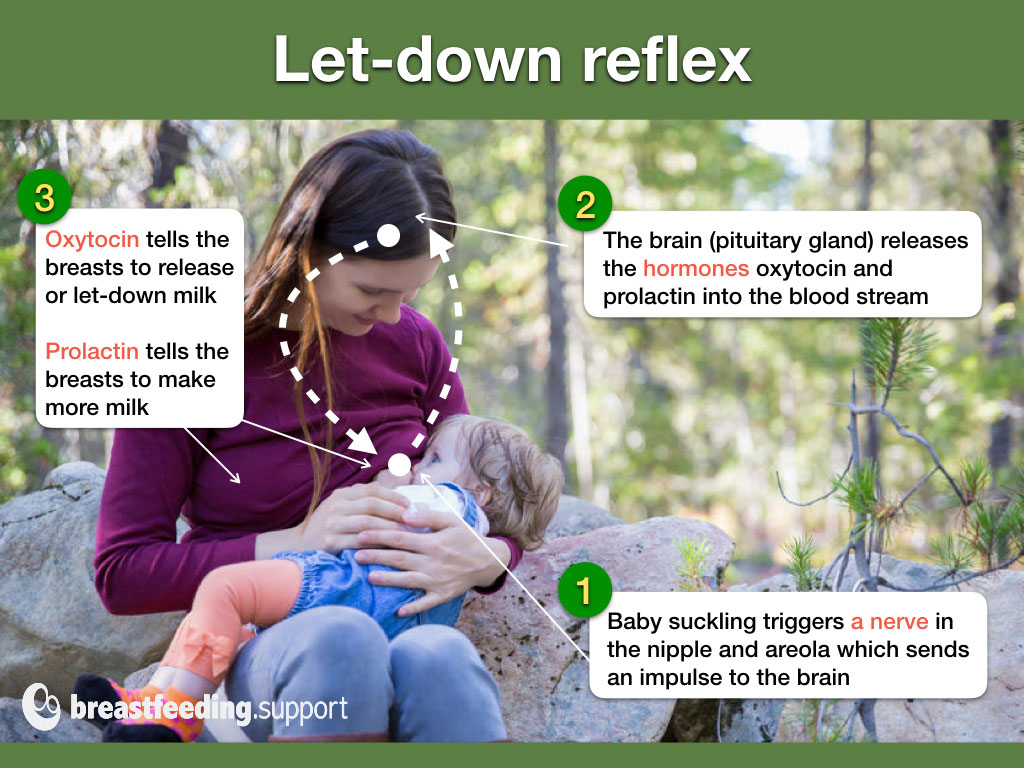
- Nerves. The fourth intercostal nerve is the main nerve providing sensation to the nipple and areola.1 Stimulation of this nerve also triggers the release of the breastfeeding hormones oxytocin (for milk release or “let-down”) and prolactin (for milk production) from the brain.2 Any damage to this critical nerve could affect the reflex needed for making and releasing breast milk.
- Milk glands and ducts. Breast milk is made inside the breast by the milk-making (glandular) tissue. Fine ducts (tubes) carry the breast milk to the nipple. Anything that cuts across or damages the ducts or glandular tissue can interrupt the exit route for milk via the nipple or the capacity of the breast to make a full milk supply. There is a greater likelihood of damaged tissues where a breast is being remodelled (a breast lift) alongside augmentation.
- Blood supply. Any major damage to the blood supply to the breast or nipple could result in local tissue necrosis (death of the tissue).
Surgical techniques
There are a number of different surgical techniques to insert a breast implant but incisions under the breast or in the armpit are thought to have less impact on milk production. Techniques include:
- Under the breast (inframammary technique) is currently the most popular technique for breast enlargement. A cut is made under the breast, and the implant is placed under the breast tissue or muscle. The scar may not be visible when the incision is in the inframammary fold or crease (where the breast meets the chest wall). This technique leaves the glandular tissue and nerves intact so has less impact on milk production.
- In the armpit (axillary enlargement or transaxillary technique). This technique involves inserting the implant under the muscle via an incision under the arm near the arm pit. Saline implants tend to be favoured under the muscle (Wambach and Spencer, 2020). Scarring is generally invisible and, as above, the technique leaves the glandular tissue and nerves intact.
- Around the nipple (periareolar incision technique) involves cutting around the nipple and areola sufficiently deeply to insert the implant packet. Cutting around the areolar minimises scarring but these incisions are associated with reduced nipple stimulation and difficulties breastfeeding.3 One study showed that women with this type of procedure were nearly five times more likely to have problems with breastfeeding due to damage to ducts, glandular tissue and nerves.4
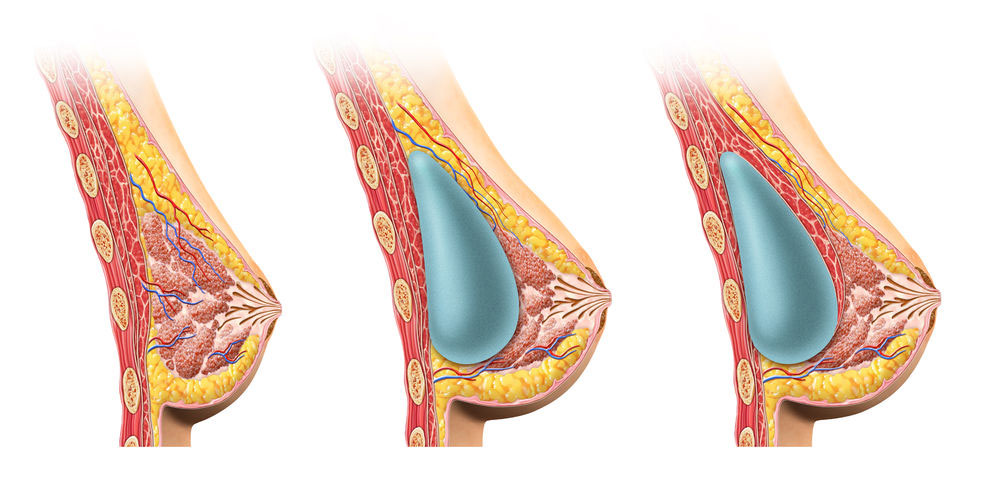
#2 Position and size of the implant
In addition to the surgical technique (#1) the size and position of the implant can affect the pressure within the breast. The breast is composed of glandular (milk-making) tissue above a layer of muscle. If the implant packet is placed between the glandular tissue and the muscle layer, it may exert more pressure on the ducts and glands which could interfere with milk flow and reduce milk production (similar to an engorged breast). Conversely, when the implant is placed beneath the muscle layer this may have less impact on milk production.5 However I have not yet found any reliable research studies discussing this assertion. Wambach and Spencer, 2020 state that the implant under the muscle allows better mammography visualisation.
Larger implants
- One study found that larger implants were associated with less nipple sensitivity after surgery6
- The larger the implant the more pressure could be exerted on the milk-making tissue
- Larger breasts can sometimes bring their own challenges to finding comfortable positions for breastfeeding see Breastfeeding With Large Breasts for more reading.
#3 Scar tissue and engorgement
Scar tissue as a result of the surgery may cause firmness in the breast, distortion and pain and can extend into milk ducts and affect the milk supply.7 If milk can’t drain freely from the breast, women with breast implants may be more prone to excessive engorgement and mastitis.8
#4 Changes to sensitivity
Following breast implant surgery some mothers find their breasts are very painful and incredibly sensitive even to normal touch making breastfeeding extremely difficult. Mothers who have had breast and nipple surgery can be more prone to experiencing nipple vasospasm (a painful, burning sensation in the nipple).9 Some mothers may have a loss of feeling or numbness in the nipple due to damaged nerves. This can affect the reflex needed for milk production and make it difficult to know when a baby’s attachment at the breast (latch) feels comfortable. If sensitivity to the nipple has been lost it still may be possible to use other triggers to initiate the let-down reflex—see Let-Down Reflex: Too Slow? by Kelly Bonyata.
#5 Functional breast tissue
Where cosmetic or reconstructive surgery to enlarge a breast is due to abnormal breast development, there may be an underlying absence of functional breast tissue. In such a situation breastfeeding difficulties could be related to this rather than the breast implant surgery directly, but problems are likely to be compounded by implants.10 Diana West discusses the breast types that are risk factors for low milk production:
Although small breast size alone is not a risk factor for low milk production, certain breast types are known to be risk factors for insufficient glandular tissue. These types include tubular-shaped breasts, widely spaced breasts (greater than 1.5 inches of flat space between them), undeveloped breasts, and asymmetrical breasts. When little glandular tissue exists to begin with, milk production capability is significantly reduced even before the surgical procedures occur.
#6 Complications
Breast implants are not lifetime devices, and often require corrective procedures.11 Complications and follow up surgery for repair or revision can cause further damage to breast tissue which can affect breastfeeding success.12 Complications can include long-term pain, hardening of the breast around the implant (capsular contracture), surgical removal of scar tissue, change of implant type, location or size, repeat breast uplift procedure, pressure within the breast and infection (Michalopous, 2007; Spear et al, 2003).
Random milk production
Occasionally a mother with breast implants may have milk production unrelated to breastfeeding (galactorrhea) or a milk filled cyst (galactocele).13 This is usually linked to postoperative congestion around the implant which often requires removal of the implants.14 Wambach and Spencer note that spontaneous milk production, milk cysts, and extreme engorgement can follow breast surgery without a pregnancy; sometimes associated with birth control hormones.15
Can damaged glands, ducts and nerves heal?
There is potential for some glands and ducts to reconnect after surgery (recanalisation) and some damaged nerves may repair themselves over time (reinnervation). How much feeling a mother has in her breasts and nipples gives a guide to whether the nerves are intact. 16
Glandular tissue itself also continues to develop under the influence of pregnancy and breastfeeding hormones and areas of the breast that are functioning normally may help compensate for any damaged areas.17 While a mother might only produce a partial milk supply for her first baby after implant surgery, subsequent babies may enjoy an improved supply. Diana West IBCLC states that the milk supply is usually better if five years have passed since the surgery (West, 2011).
Maximising milk supply
If you are breastfeeding with implants it may be helpful to stay in close contact with an IBCLC lactation consultant for support. You can also read our articles on getting breastfeeding off to a good start, increasing milk supply and the value of galactagogues (herbs, foods or medications that may promote milk production).
Safety issues
What are implants made of?
Most breast implants comprise a silicone shell filled with silicone gel (made from silicon) and some are filled with saline (salt water). Silicone is a synthetic substance, a mixture of compounds made from silicon (a naturally occurring element found in sand). In manufacturing, silicone is generally described as having low toxicity and has various uses in industry (insulation sealants), in the medical field (tubing), and in the home (kitchenware, bottle teats, toys). Within the human breast itself however, silicone has been associated with many health issues.18
Risks and complications of breast implants
The general safety of breast implants is beyond the scope of this article, for further information see:
- What You Need to Know About Breast Implants, by the National Center for Health Research.
- Breast Enlargement (Implants) from United Kingdom’s National Health Service (NHS).
- Risks and Complications of Breast Implants from the U.S. Food and Drug Administration (FDA).
- Breast Implants and Anaplastic Large Cell Lymphoma (ALCL) (UK gov) updated 27 March 2025.
- Silicone Breast Implants and Injections updated January 2025.
- Healing Breast Implant Illness and Breast Implant Illness—are support groups offering support and information to those experiencing symptoms of breast implant illness which includes autoimmune disease, cancer and more.
- New research provides a possible mechanism for breast implant illness from gel-filled silicone implants.19
There is concern that breast implants can cause lactation difficulties, reproductive problems and adverse medical conditions2021
Is breastfeeding with implants safe?
The safety of breastfeeding with implants is unclear:
- Conflicting information. In the USA, the Centers for Disease Control and Prevention states that there is insufficient evidence to say breast implants can harm a breastfed baby.22 Conversely one support group has collected studies, mostly from 1990s, that indicated possible harm for some children born or breastfed by mothers with implants.23 Thomas Hale, breastfeeding and medications expert, says silicone is inert (chemically inactive) and unlikely to be absorbed in the gastrointestinal tract by a breastfed baby although he cautions good studies are lacking.24
- Gaps in knowledge. Research has found that when silicone devices are inside the body they have the potential to trigger inflammation and health issues.25262728 How this could affect a foetus or breastfed infant is not clear and more long-term studies are needed.
Can breast implants leak into breast milk?
The Food and Drug Administration of the United States say it is not known whether small amounts of silicone from breast implants can enter breast milk:
At this time, it is not known if a small amount of silicone may pass through from the breast implant silicone shell into breast milk during breastfeeding. Although there are currently no established methods for accurately detecting silicone levels in breast milk, a study measuring silicon (one component in silicone) levels did not indicate higher levels in breast milk from women with silicone gel-filled implants when compared to women without implants.
The “study” often cited by Semple et al 29 is from nearly 30 years ago and was published in a plastic and reconstructive surgery journal (so potentially biased). It found similar levels of silicon in breast milk and blood from mothers with implants compared with mothers without implants. They also found ten times more silicon in cows’ milk and significantly higher levels in formula. However, silicon is not the same as silicone—it is an ingredient in silicone and the study didn’t look at the other potential toxic contaminants that are in implants. A study by Lykissa and Maharaj 30 found higher levels of platinum in mothers’ milk in mothers with implants than in the general population.
Hyaluronic acid injections
Core Curriculum for Lactation Consultant Practice, 2013 says that hyaluronic acid injections (Macrolane) directly into breast tissue, have been used to increase breast size since 2008. Regarding their safety with respect to breastfeeding they state:
Hyaluronic acid injections are not a contraindication to breastfeeding. The oral bioavailability of hyaluronic acid is nil and therefore even if it were to transfer into milk, it would not be readily absorbed by the baby’s GI tract (Hale, 2010; infantrisk.com, March 2011)
Summary
Breast implants have the potential to compress milk ducts and affect milk flow which can reduce a milk supply. The surgical technique used during the procedure and how much functional glandular tissue was present prior to the surgery will also dictate exactly how milk supply is affected. With these potential difficulties in mind, a mother breastfeeding with implants should take extra care to get breastfeeding off to a good start so she can maximise her milk supply. An IBCLC lactation consultant is a helpful partner to have especially if there are any early signs that baby is not getting enough milk or not gaining weight normally. It is not known whether silicone from the breast implant packet can enter breast milk. Until research proves otherwise, babies are still thought to benefit from any amount of human milk that can be provided. Currently there is no clear evidence that breastfeeding with implants could harm the baby directly other than by reducing milk available but more long-term studies are needed.
Given the risks of complications, women would be wise to delay implants until after they have their children and are no longer breastfeeding.