Making breast size smaller in a surgical procedure is known as breast reduction. This article discusses how breast reduction surgery can affect milk supply, whether women who have had breast reduction surgery can still breastfeed and answers frequently asked questions. For information about breast augmentation see Breastfeeding With Implants.
Breastfeeding after breast surgery
To make breast milk, a breast needs glandular or milk-making tissue and a neurohormonal reflex to release the milk (see box). Any kind of surgery on the breast has the potential to disturb milk production or milk release to some degree. How breastfeeding might be affected after breast reduction surgery will depend on:
- The type of surgery involved—whether important nerves and milk ducts (tubes that carry milk to the nipple) have been cut, whether the nipple has been repositioned, and whether the blood supply to the breast is intact.
- How much milk-making (glandular) breast tissue remains
- The length of time since the surgery
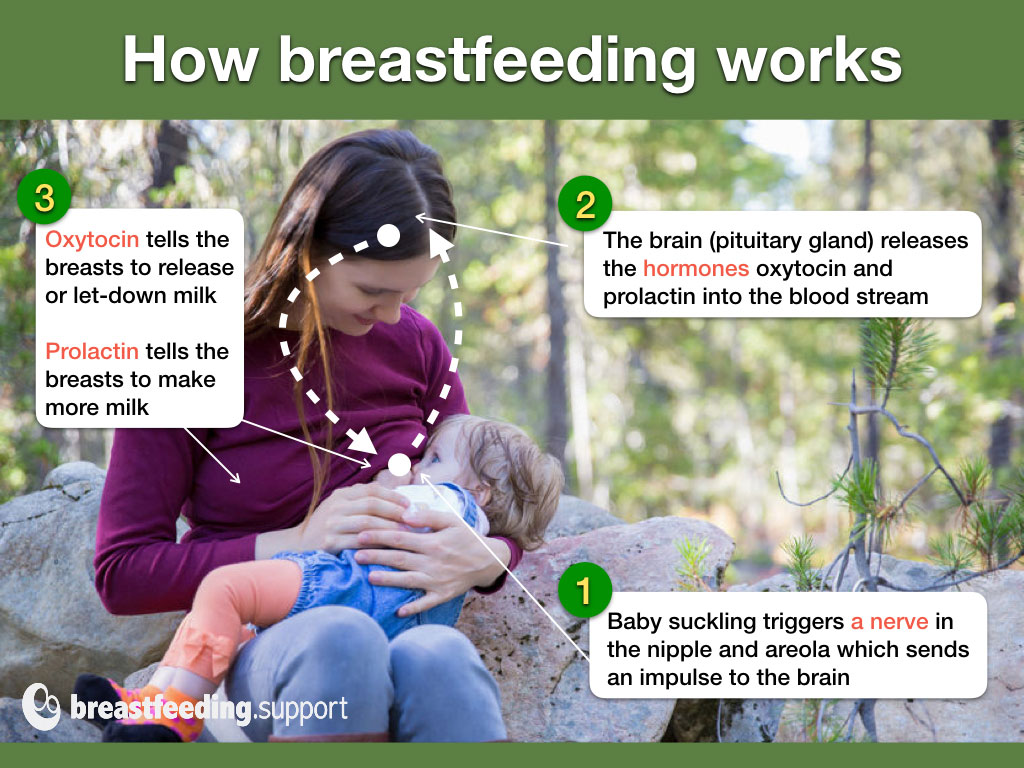
How breastfeeding works. A baby’s suckling stimulates a nerve by the nipple to send a message to the brain to release specific hormones (oxytocin and prolactin). Oxytocin signals breast milk to be released (let-down) from the milk-making tissue in the breast so that the milk is carried to the nipple through little tubes (ducts). Prolactin signals milk production. Any damage to the nerves, ducts or glandular tissue can affect how breastfeeding works after breast reduction surgery.
#1 Type of surgery
During breast reduction surgery part of the breast will be physically removed and this could affect milk supply in a number of ways:
- Cutting across important nerves can reduce nipple sensitivity and affect the neurohormonal reflex that triggers milk production and let-down.
- Cutting through milk ducts means that areas of the breast may become engorged and ultimately shut down milk production because there is no outlet for the milk.
- If the nipple is removed and then placed on a reconstructed breast, the resulting damage to the nerves, milk ducts, and breast tissue will affect breastfeeding significantly.
- Scarring inside the breast may affect lactation. The scar pattern on the surface of the breast does not reveal the type of surgery.
Surgical techniques
Several surgical techniques are possible for breast reduction and some will have more impact on breastfeeding than others. The best chance for breastfeeding success will be where the procedure leaves the nipple and areola attached to the breast tissue beneath them. Lactation consultant Diana West has outlined a selection of techniques in her book Defining Your Own Success Breastfeeding After Breast Reduction Surgery and these are summarised below:
- Fat removal (liposuction). Cuts are made in the breast to insert a suction tube to remove fat deposits from areas of the breast. This may damage glandular tissue depending where the tube is inserted, and may cause scarring but is thought to be the least damaging technique for breastfeeding.
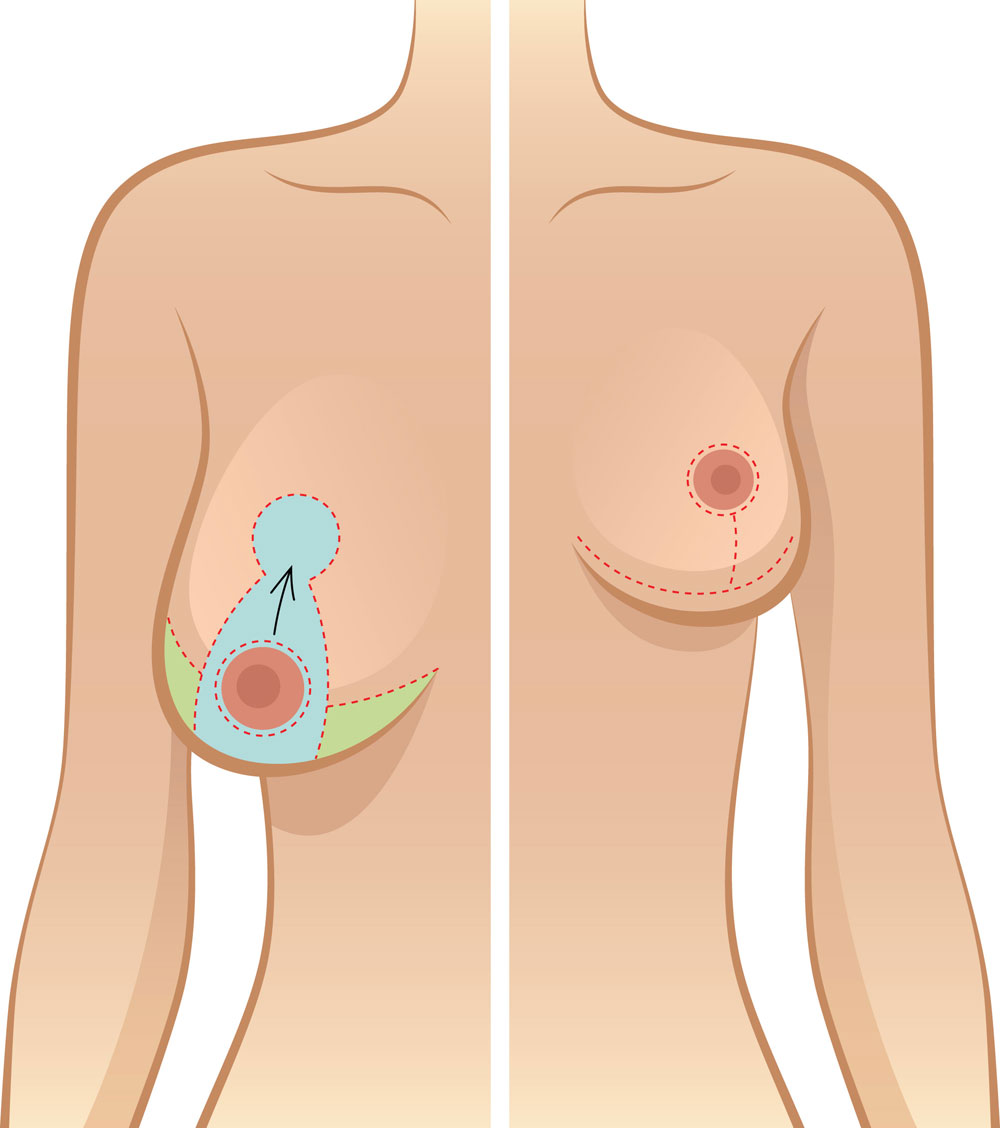
- Anchor type or inverted-T (inferior pedicle technique) involves removing sections of the breast and repositioning the nipple. The nipple is left on a mound of tissue (pedicle) so that it still has its nerves, blood supply and ducts intact. More glandular tissue may be retained with this technique compared to others which helps to preserve some degree of breastfeeding later. The surgery leaves a scar running around the areola (the darker skin around the nipple), a vertical scar from nipple to the chest wall, and then a horizontal scar under the breast in the crease where the breast meets the chest wall (inframammary crease or fold) making an anchor shaped scar.
- Around the areola (periareolar) technique involves making an incision around the areola and pulling out breast tissue through the incision. Glandular tissue will be removed along with fatty tissue and important nerves may be damaged.
- Central mound technique preserves the nipple and areola. However there is likely to be considerable damage to the glandular tissue due to the specific methods involved in reshaping the breast.
- Periareolar with mesh support (or “double skin”) involves a similar technique to the periareolar technique above however a synthetic mesh is inserted in the breast to provide support and reduce post surgery sagging. The technique can remove large amounts of glandular tissue and important nerves may be damaged.
- Superior pedicle technique (or “Lejour”) preserves the nipple-areola complex but can impact on the nerves and ducts as it removes a significant amount of glandular tissue directly below the nipple.
- Free nipple graft involves complete removal of the nipple and grafting it back to a new location on the remodelled breast. All nerves and ducts will be severed causing significant damage to breastfeeding and affecting nipple sensation. Even though establishing a milk supply is unlikely, it is possible for some nerves and ducts to reconnect and some sensitivity to return.1
#2 How much glandular tissue remains?
Glandular tissue in the breast is interspersed with fatty tissue and it is not possible to say by just looking at the size of a breast how much glandular tissue is present before or after surgery. Therefore we can’t assume a large breast has more glandular tissue than a small breast or that a large breast can afford to be halved by surgery and still be functional. How breast reduction can affect milk-making capacity depends on how much functional glandular tissue is left after surgery. The more glandular (milk-making) tissue that is removed by surgery, the more likely it is that breastfeeding (milk supply) will be affected.
#3 How much time has passed?
As time passes after breast reduction surgery, damaged nerves may reconnect (reinnervation) and severed ducts may make new connections to the nipple (recanalisation). Nipples that had lost any sensitivity may become more sensitive again and the capacity of the breast to make milk may improve.
Healing of milk ducts (recanalization)
Some milk ducts that have been cut or damaged seem to reconnect or develop new pathways to carry the milk to the nipple. The hormones of pregnancy and to an extent the menstruation cycle can also help with development of new glandular tissue. Breastfeeding also helps this process—with each new breastfeeding experience there can be a little more recovery and a better milk supply. Recovery will be limited by how much breast tissue and how many milk ducts remain intact.
Healing of nerves (reinnervation)
An important nerve for triggering the release of prolactin and oxytocin is the fourth intercostal nerve. If this is damaged it affects let-down and milk production. According to bfar.org, a website dedicated to breastfeeding after breast reduction, damaged nerves can take about five years to grow back to significant or full function.2 A good sign that this is happening will be when any lost sensitivity to touch and temperature returns to the nipple.
Frequently asked questions
Will I have enough milk?
Although some women manage to breastfeed successfully, there is a strong possibility that you won’t have a full milk supply, especially for the first baby born after breast reduction surgery. It will be important to keep a close eye on your baby’s weight gain and nappy output to gauge their milk intake. It may be necessary to supplement your baby. An IBCLC lactation consultant can help you optimise your milk supply and see A Good Start to Breastfeeding and Is My Baby Getting Enough Milk?
What if supplements are needed?
It’s important that your baby is well fed to give them enough energy to breastfeed and prevent jaundice or dehydration, so supplements of donor milk or formula may be needed. Although you may not be able to make a full supply of milk, any amount of breast milk you can provide will be beneficial to your baby. Breastfeeding is a relationship, not just a way to feed a baby, so comforting your baby at the breast and holding your baby in skin-to-skin contact will be valuable even if you don’t have much milk.
If you need to supplement, options include:
- A supplemental nursing system. This allows a mother to supplement her baby directly at the breast using a feeding tube, see photo below and Breastfeeding With a Supplemental Nursing System
- Finger feeding. Top ups to supplement breastfeeding could be offered short term by finger feeding see What is Finger Feeding?
- Bottle. There are lots of ways to make a bottle feed more like a breastfeed so that a baby doesn’t get confused by switching between breast and bottle see our Tips to Bottle Feed a Breastfed Baby and Best Bottle for a Breastfed Baby.

How can I maximise my milk supply?
See A Good Start to Breastfeeding and Breastfeeding Tips for Newborns for general ideas to get breastfeeding working well and see our tips below:
Before the birth
Discuss thoughts on antenatal expression of colostrum with your health professionals and see Expressing Colostrum Antenatally.
The first hour
Spending time in skin-to-skin contact and breastfeeding in the first hour after birth has many advantages for mother and baby including helping a milk supply. If baby isn’t ready to latch on, hand expressing can remove milk instead of baby. This video by Jane Morton explains why the first hour is important for milk supply: A Mother’s Touch Breastfeeding in the First Hour.
Frequent feeds
Frequent breastfeeding or hand expressing (at least every two hours, more if you can) will help stimulate your milk supply. It may be useful to pump after breastfeeds for a few weeks once your milk is in to maximise your supply.
Comfortable breastfeeds
Ensure breastfeeding doesn’t hurt, see Latching Tips and Breastfeeding Positions for Newborns.
Making more milk
There are lots of ways to increase a milk supply including frequent pumping with a hospital grade pump, using both breasts per feed, breast compressions, and frequent feeds. It can be very useful to see an IBCLC lactation consultant to help you as there can be other Reasons for Low Milk Supply, not just the surgery. See How to Make More Breast Milk and How to Increase Milk Supply by Pumping.
Galactagogues
A galactagogue is a food, herb or drug that might help to increase milk supply or help promote more glandular breast tissue. For much more information see What Is a Galactagogue?

What difficulties might I expect after surgery?
Certain difficulties may present themselves if you have had breast surgery. But bear in mind these problems can come along at any time and may not be to do with the surgery at all—check with an IBCLC lactation consultant or breastfeeding specialist.
Severe engorgement when milk comes in
Some breast engorgement (feelings of fullness and swelling) after birth is normal. Engorgement is not just from milk but includes tissue fluid and blood in the breasts. Engorgement is a good sign that functional milk-making tissue is still present. However some milk ducts may be blocked due to the surgery or scarring. One breast may be more engorged than the other. Areas of the breast that are not able to drain will shut down milk production. Engorgement may be worse with second and subsequent babies particularly after a long and successful breastfeeding experience previously. Try to remove as much breast milk as possible to relieve the engorgement and see Engorged Breasts, and Engorgement Relief When Milk Won’t Flow.
No engorgement when milk comes in?
There can be several reasons for milk not coming in after delivery in addition to removal of glandular tissue by breast surgery. See No Breast Milk After Delivery and contact an IBCLC lactation consultant for help and support.
Reduced nipple sensation
If you do not have any sensitivity in your nipples it can be harder to initiate the let down, but there are ways to condition this response to other triggers, see Let-Down Reflex: Too Slow? by Kelly Bonyata.
Nipples painful, sore, or white
Mothers who have had nipple or breast surgery are more at risk of nipple vasospasm (sudden narrowing or constriction of blood vessels in the nipple accompanied by pain). This is perhaps due to trauma to the blood supply and nerves (bfar.org, 2022). As nipple vasospasm can have other causes such as poor attachment, positioning, certain drugs—including caffeine and nicotine—or Raynaud’s Phenomenon, it is important to rule out all causes. See Nipple Vasospasm and Breastfeeding for more information on treatments and prevention and check wth your breastfeeding helper.
Pain in the breasts
Adhesions in the breast (scars) may be a cause of pain and may inhibit the let-down. There are other causes of pain to rule out however. Engorgement, mastitis, mammary constriction syndrome and a shallow latch can create deep breast pain.
When an adhesion is suspected, the first remedy is to try to move the layers of tissue by frequent, gentle massage, which will break the adhesions if they are not too dense. In the case of nipple adhesions, the nipples can be gently pulled outward. With time and active use of the breast, the adhesions will usually diminish in severity.
Considering breast reduction surgery?
Breast reduction surgery can cause difficulties breastfeeding and many women will not be able to breastfeed. If you have not already had breast surgery you will want to consider this fact alongside the other medical risks3. Breastfeeding may not seem important to you now, but this might change when you approach motherhood. Although there are ways to minimise the impact on breastfeeding when performing surgery this is not a guarantee to success and not all breast surgeons consider protecting breastfeeding without prompting.
What should the surgeon say to the woman asking for breast reduction surgery? That the chances that she will be able to breastfeed her babies exclusively are low. And if this woman is 16 or 17 years old, maybe it’s better to wait a few years, because the surgery cannot be undone, and perhaps in a couple of years she may have a different outlook on life.
The surgeon should clearly discuss the options with the patient or provide a procedure that leaves the ducts intact. If the ducts are intact, breastfeeding can be successful postoperatively. The nerve must also be intact for tactile sensations to trigger let-down.
Support groups
Good support can be essential for maximising your milk-making potential. Contact an IBCLC lactation consultant for one-to-one help and for online community support visit Breastfeeding After Reduction (BFAR) and BFAR UK Support Group (Facebook groups).
Summary
Breast reduction surgery can present several challenges for breastfeeding. However a mother may be able to make a full or partial milk supply depending on the type of surgery, amount of functional breast tissue removed and the time that has passed since surgery. It is important to make sure breastfeeding gets off to a good start to maximise a milk supply after a surgical procedure. An IBCLC lactation consultant or breastfeeding specialist is an ideal support person to help with this so that any breastfeeding problems unrelated to your surgery can be ruled out and your breastfeeding potential can be maximised.