When a mother meets all her baby’s nutritive needs via pumped milk it is known as exclusively pumping breast milk. Exclusive pumping may happen when a mother makes a choice to express her milk for her baby instead of breastfeeding or it may be a temporary situation if a baby can’t breastfeed straight away. Although there are lots of ways to help a baby back to the breast, sometimes, even with good help, a mother may find herself pumping her breast milk temporarily or long-term. This article answers frequently asked questions about exclusively pumping breast milk whether as a choice or because breastfeeding has not worked out. This is a companion article to How to Increase Milk Supply When Pumping.
Why exclusively pump breast milk?
Exclusively pumping:
- Avoids using industrially made formula so preserving biologically normal health for mother and baby.
- Protects a milk supply until direct breastfeeding can be established later.
- Can help with the grief, frustration or feelings of loss when breastfeeding doesn’t work out.
- Provides flexibility for others to feed baby when mother and baby must be separated.
- Avoids ongoing costs of buying formula because breast milk is free.
Are there any disadvantages?
- Exclusively pumping is usually harder than breastfeeding. It can feel very time consuming and overwhelming to pump, bottle feed and sterilise equipment while juggling a hungry baby.
- Being tied to a pump at regular intervals can be limiting especially when away from home.
- Mothers may still grieve for the loss of breastfeeding and not being able to calm a baby at the breast.
- Although a baby will get all the benefits of breast milk, not breastfeeding may increase the risk of overfeeding1 (paced bottle feeding can help with this), or increase the risk of suboptimal oral development23.

How is breast milk made?
Milk making tissue develops in the breasts during pregnancy. Colostrum (the first breast milk) is quite thick and sticky and low in volume and is already present in the breast before baby is born.
What controls breast milk production after birth?
- Hormonal control. The delivery of the placenta at birth, and the sudden drop in the hormone progesterone, signals the mother’s breasts to start making a higher volume of breast milk. The production of colostrum and this initial triggering of full milk production happen automatically whether or not you put your baby to the breast or plan to breastfeed. Mothers usually feel their milk “come in” around the second or third day after birth. You may hear this process referred to as hormonally driven (an endocrine process).
- Effective milk removal. After the milk volume initially comes in, continued milk production depends on frequent removal of milk from the breasts. The hormones prolactin and oxytocin must still be present for milk production, but the main influence on milk volume is how quickly the breasts are emptied. You may hear this described as locally controlled in the breast (autocrine control). If milk is not removed from the breasts, milk production shuts down.
What does this mean for exclusively pumping mothers?
Mothers will need to express their breast milk as often as a breastfed baby would normally feed or as often as needed to maintain a full milk supply. Pumping regularly throughout the day and at least once at night helps to maximise breast milk production and ensure a good breast milk supply. See How often should I express my milk? below for more detail.
Types of breast pump
Breast pumps vary a great deal in their efficiency, portability and cost and tend to fall into four groups:
- Manual pump—Types include those operated by squeezing a lever with the hand to maintain suction on the breast and one piece silicone pumps e.g. Haakaa that work by attaching to the breast by suction. Usually the cheapest types of pump.
- Single electric breast pump for pumping one breast at a time. Different models may vary widely in quality.
- Double electric breast pump—allows pumping both breasts at the same time which is desirable for exclusively pumping. Portable hands-free double and single pumps allow the user to move around while pumping. Some pumps are wireless, cordless and/or controlled via an app from a smart phone.
- Hospital grade double electric breast pump—a pump with a stronger motor suitable for more than one user and with a greater reliability and efficiency. Although expensive to buy, they can be hired from pump manufacturers.
What is the best type of breast pump for exclusively pumping?
For exclusively pumping, a double electric breast pump or ideally a hospital grade pump are usually the most effective breast pumps. However since breasts come in many different shapes and sizes, different pumps suit different mothers so bear in mind that what works well for one mother may not be quite right for you. Note that pumping should not be painful; if it is painful this is likely to be counterproductive.
Flange size
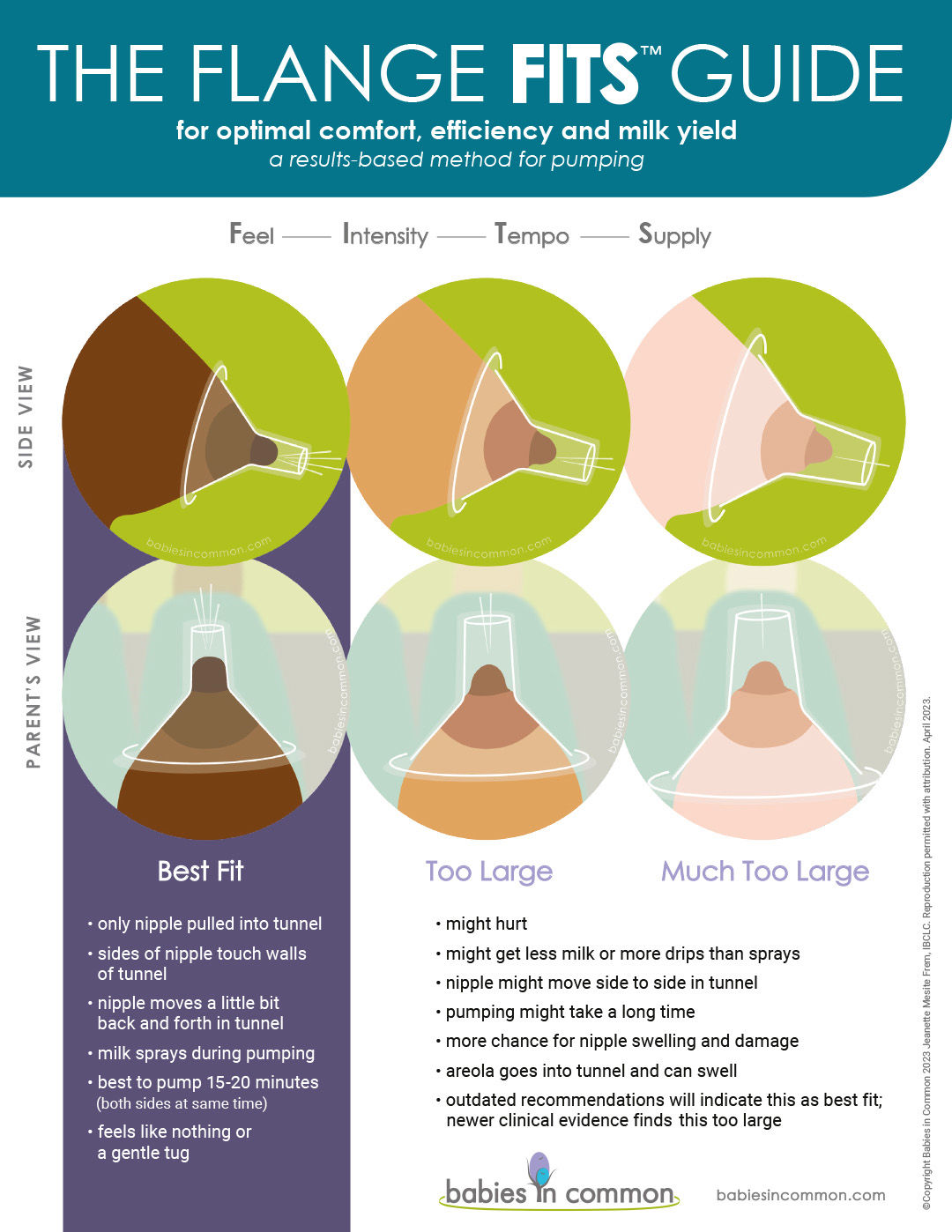
It is important to use correctly sized flanges (the part of the pump that is held next to the breast) so that pumping is both comfortable and effective. A useful resource is The Flange Fits™ Guide from Babies in Common.
Choosing a pump
Look for a pump with multiple settings for speed and suction, a range of flange sizes and good reviews. Breastfeeding authors Lisa Marasco and Diana West highlight a selection of popular pumps and their individual features at lowmilksupply.org. For more tips including why a second hand pump is not usually a good idea, how to clean pump parts and more about flange fit see How to Increase Milk Supply When Pumping.

When should I start pumping?
It is important to start expressing colostrum as soon as possible after the birth if your baby can’t latch or you have chosen to pump. Research suggests within an hour is beneficial45 and certainly within six hours. Studies indicate hand expressing combined with pumping yields best results in the early days after birth.6
How often should I express my milk?
Eight to ten times per day
Try to pump at least eight to ten times in 24 hours in the first few weeks.7 Frequent and thorough milk removal in these early days and weeks helps ensure a full milk supply later.8 Frequent feeds also mimic a baby’s breastfeeding pattern—a baby feeds very frequently, has a small tummy and can digest breast milk in an hour. Pumping and/or hand expressing for 10-15 minutes every two to three hours around the clock is a good guide for the first few days after birth9 and then continuing on a similar schedule but pumping long enough to thoroughly empty the breasts after milk comes in (see below). Avoid any long stretches of five or six hours between expressing sessions (apart from one longer stretch at night if everyone is sleeping) and try to pump at least once during the night (Mohrbacher 2020).
Storage capacity will affect pumping frequency
The amount of breast milk a breast can store between feeds is known as the storage capacity and depends on the amount of glandular tissue (milk making tissue) in any particular breast. Breasts with a smaller storage capacity can make just as much milk in 24 hours as those with a larger capacity but will need to be emptied more frequently. Therefore a mother with a small storage capacity will need to pump more often. A mother can gauge her pumping frequency by her overall volume pumped. If she needs more breast milk she can try pumping more often, for less breast milk she can reduce her pumping frequency.
Pumping patterns may change
Storage capacity may continue to increase in the first few months10 which may help explain why pumping patterns can change over time. Once a mother’s milk supply is well established she can often go longer between pumping sessions without affecting her overall milk volume. After milk supply is at full production, Nancy Mohrbacher, breastfeeding author and IBCLC lactation consultant, refers to the perfect number of pumping sessions for an individual mother as the “magic number”:
The “magic number.” This refers to the number of times each day a mother’s breasts need to be well drained of milk to keep her milk production stable. Due to differences in breast storage capacity, some mothers’ “magic number” may be as few as 4-5 or as many as 9-10. But when a mother’s total number of breast drainings (breastfeedings plus milk expressions) dips below her “magic number,” her milk production slows.
Do I need to pump at night?
If you are exclusively pumping it is important to express breast milk at night in the first few months after your baby is born to stimulate a full milk supply. Prolactin is an important hormone involved in milk production and it has naturally high levels at night11 making this seem a good time to fit in a pumping session. Leaving breasts full all night is likely to slow down milk production.
How much milk do I need to pump if I am exclusively pumping?
After the first week or two, a baby’s average requirement for breast milk is around 750-1035 ml or 27-35 oz12 or an average 800 ml/day 13 and this volume remains fairly constant from months one to six. Aiming to pump a volume that just exceeds this average will provide a cushion for growth spurts. Mothers of twins will need to aim for double this volume.
How long should I pump at one time?
Pumping time will vary depending on the type of pump used, whether you’re pumping exclusively to build a milk supply or pumping occasionally alongside breastfeeding. A mother with a small breast storage capacity will need to pump for a shorter time more frequently compared to a mother who stores more milk at one time making the process very individual to each mother.
Twenty minute starting point
Nancy Mohrbacher suggests pumping for twenty minutes for a few sessions while observing milk flow and then adjusting the time pumped as required: simply pumping for a longer or shorter time as needed to remove all the milk (Mohrbacher, 2020. p 490). The goal is to establish a full milk supply (750-1035 ml per day) by 10-14 days after the birth. Once the goal is met, pumping length may return to 10-15 minutes for some mothers.14
Watch milk flow rather than the clock
In their study, Morton et al found a double pumping session including all the steps in the next section averaged 25 minutes. However the authors point out that specifying an ideal time to pump may not be helpful as some mothers were pumping for 15 minutes and others for 45 minutes15. The 2010 edition of The Womanly Art of Breastfeeding had a good summary:
A pumping session that replaces a nursing will probably last no more than fifteen minutes if you’re double pumping or about twenty minutes if you’re single pumping. Don’t watch the clock to know when your pumping session is over—feel your breasts to see if they’re lighter and softer. If you can’t tell, begin by pumping for fifteen to twenty minutes paying attention to how your breasts feel. When you know your breasts better you’ll know when to stop.
Total pumping?
One resource states that a total of 120 minutes of pumping per day is a good rule of thumb16 while Morton et al refer to a daily pumping time of around 150 minutes albeit with the caveat mentioned above (Morton, 2009). However because of individual variation between breasts it is not really possible to specify a time limit. The total number of separate pumping sessions is more important than pumping length per session and sessions don’t need to be equally spaced throughout a day (Mohrbacher. 2020. p 502) Shorter, more frequent pumping sessions are likely to be more productive overall than fewer, longer sessions.
How can I increase my milk supply when exclusively pumping?
This section should be read in conjunction with How to Increase Milk Supply When Pumping.
Getting started
Oxytocin is the hormone needed to cause your milk to “let-down” (milk ejection reflex) to your baby or a pump. When breastfeeding, the let-down is triggered by sucking when a specific nerve alongside the nipple is stimulated in a neurohormonal reflex. Hearing your baby cry, holding your baby skin-to-skin or looking at your baby can also trigger this reflex. Tips to initiate the let-down when pumping include:
- Warmth. Mothers have found that taking a warm shower or using warm compresses to the breasts can help trigger a let-down. Warmth is also associated with a higher volume of milk 1718
- Massage. Before (and during) a pumping session, gently massaging the breasts can help to prepare the breasts and to initiate the let-down. See The Basics of Breast Massage and Hand Expression, a video by lactation consultant Maya Bolman.
- Hand expressing. Initiating the let-down before pumping by a combination of a gentle stroking massage and hand expressing works well for some mothers.
- Conditioning the let down. The let-down reflex can be conditioned into an automatic reflex by establishing familiar routines for example sitting in the same place, and listening to the same music as you pump. The smell of your baby, looking at your baby or having a photograph of them or even thinking about your little one can all be helpful triggers.
- Relax, avoid stressors. Stress, embarrassment, feeling rushed, feeling cold, or experiencing pain from a poorly fitted pump flange could all hinder a let-down to the pump. In addition smoking, caffeine, alcohol, and some medications can affect the let-down or impact on volumes pumped for some mothers.
- Music. Listening to music may produce more milk with a higher fat content1920.
- Pain free. Use a good breast pump and ensure the pump flanges are the correct size and that pumping is comfortable and without pain.
- Use lubrication inside the pump flange to reduce friction if needed. Some mothers use nipple creams such as lanolin, oils (e.g. olive oil or coconut oil), or even breast milk. Note that some authors point out that lubrication shouldn’t really be needed with a well fitted pump.21
- Centre each nipple in the nipple tunnel of the pump flange and ensure there is contact with the breast all around the shield to make a comfortable seal without pressing hard into the breast.
During pumping
- Pump settings: suction (vacuum) and speed (cycles). Recommendations vary slightly between different authors and mothers will need to experiment to find what combination of vacuum and speed works best for them. One author says use the highest comfortable vacuum setting that maintains milk flow, start with a high speed to trigger milk ejection, decreasing speed once milk flows then returning to a faster speed to trigger another milk ejection when flow slows down and then repeat (Mohrbacher, 2020 p490). Another says start with a low suction and high number of cycles to trigger the let-down. Once milk lets-down and starts to flow, decrease the cycles and increase suction enough to maintain flow (Casemore, 2014 p89). Taking a short break during pumping to grab a tea or coffee and come back to the pump can also work for some mothers.
- Double pump. Pumping both breasts at the same time can help with milk production2223. If you are single pumping try switching between breasts—pump each breast for five minutes and then repeat.
- Massage the breasts and/or use gentle breast compressions during pumping (often called hands on pumping) to help increase milk volume. A double pumping bustier can hold the flanges in place to free the hands to massage each breast in turn or it may be more effective to pump breasts one at a time. It is important to be gentle with any breast massage using only a light touch—similar to stroking a pet or applying cream to the skin—to avoid causing inflammation or bruising of the breast tissue. There is more information about breast massage in Hand Expressing Breast Milk and see What is Breast Compression? One study showed a daily increase of breast milk volume of 48% with hands on pumping24. In addition, using hands to massage the breasts also seems to increase the calorie content of pumped milk—an important advantage for premature babies25. See Jane Morton’s Hands on Pumping video (watch from 5:15) from Stanford University for more information.
- Stop pumping and massage. Once milk stops flowing and there are only drops of milk appearing, stop pumping and gently massage both breasts (Morton, 2009).
- Finish by hand expressing or using a single breast pump alternating from the left to right breast and repeating until both breasts are fully drained (Morton, 2009). Hand Expressing Breast Milk has more information on hand expressing techniques.
Keeping a record of volumes of milk pumped per session and per day can be a good motivator to encourage you and see How to Increase Milk Supply When Pumping.

Troubleshooting
Not enough milk
If after following all the steps and tips above your milk supply is still lower than your baby’s needs:
- Check whether your breast pump is working properly and is completely comfortable. Pump parts affecting suction may need replacing after six months26. Consider hiring a hospital grade pump or trying a different style pump and see How to Increase Milk Supply When Pumping.
- Try pumping more often. “Power pumping” or “cluster pumping” are names coined to correspond to how a baby feeds frequently during a growth spurt or bursts of cluster feeding. Try variations of pumping in short bursts e.g. pump for 5-10 minutes then rest for 10-15 minutes and repeat for blocks of time each day. Some pumps have power pumping features built in eg Ardo’s Alyssa.
- Try holding your baby skin-to-skin as much as possible to stimulate your hormones.
- Try pumping more often in the night when prolactin levels are higher.
- Diet. See Best Breastfeeding Diet and Foods to Avoid for more information.
- Check whether any medications you might be taking could be affecting your milk supply including hormonal contraceptives, antihistamines, certain herbs e.g. sage, peppermint, even placenta tablets. Sometimes the return of a mother’s periods can cause a temporary drop in supply.
- Find out more about galactagogues (food, herbs or drugs thought to increase the production of breast milk). See What is a Galactagogue?
- Medical causes. Consider whether there are any reasons for low milk supply in your medical history that you could discuss with your doctor or lactation consultant.
Too much breast milk
Some engorgement when a mother’s milk first comes in around three days after the birth is quite normal and doesn’t necessarily indicate oversupply (too much breast milk). This engorgement is partly due to blood and tissue fluids in the area as well as breast milk. For more information on how to handle this early engorgement see Engorged Breasts. After the first couple of weeks, breast milk production will normally settle down to a volume that exactly balances the amount of milk removed from the breasts. Sometimes however, a mother might feel constantly full of milk, leak between pumping sessions and seem to pump over and above her baby’s needs until she has a freezer full of frozen milk. Some mothers will need to take steps to reduce their supply a little. The different strategies for reducing supply are described in Oversupply of Breast Milk and the principles can be applied to the exclusively pumping mother.
Reducing a milk supply when pumping
A mother who is exclusively pumping can reduce the length of each pumping session to slowly regulate her supply, or begin to space the pumping sessions a little further apart. Some mothers consider herbs and medications to help reduce a milk supply, see Too much milk: Sage and other herbs for decreasing milk supply by Kelly Bonyata for further reading. Whenever a breast is full, milk production will slow down so over time the strategy of having fuller breasts between sessions will down regulate the milk supply. However, go slowly, it is very important to always pump enough milk to remain comfortable to avoid blocked ducts or mastitis (breast inflammation).
Sore nipples
Pumping should be comfortable and not make a mother’s nipples sore. However a poorly fitted pump flange rubbing a nipple, a suction that is too high, not using lubrication or a poor quality breast pump could cause pain and friction during pumping leading to sore nipples. Occasionally a mother could have a skin reaction to the plastic used in the pump flange 27 Whenever skin has been broken around the nipple or base of the nipple there is a higher chance of getting an infection. For further reading see:
- How to Increase Milk Supply When Pumping has information on breast pump flange fit
- Treatments for Sore Nipples
Blocked ducts and mastitis
A mother who is pumping exclusively can run into a number of difficulties just as a breastfeeding mother can. Breast lumps due to engorgement, blocked ducts or mastitis have many causes including:
- Missing a pumping session so that breasts become painfully engorged
- A pump that is not draining all areas of the breast thoroughly—gentle breast massage during pumping may help with this and check whether you are using the pump correctly and that the pump flanges are centred on the nipples and are a good fit.
- Rough handling of the breast for example through too firm breast massage or breast compressions.
- Any pressure on the breast; check whether your nursing bras are a good fit for you.
For more information see Engorged Breasts, Blocked Milk Duct and Mastitis Symptoms and Treatment.

How long can I store breast milk?
For much more information about storing breast milk see How Long Does Breast Milk Last?
Premature baby?
If you’re exclusively pumping for a premature baby see Breastfeeding a Premature Baby, and Kangaroo Care for Your Premature Baby for much more information.
When can I drop pumping sessions?
The number of pumping sessions needed to maintain the right volume of milk for a mother’s baby is individual to each mother and varies with breast storage capacity and a baby’s needs. In the early weeks frequent pumping throughout the day and not forgetting at least once at night are the key to a good long term supply. As time goes on however, after a full supply has been established, many exclusively pumping mothers find they can reduce the number of pumping sessions and still get the same volume of milk per day overall. In her book Exclusively Pumping Breast Milk author Stephanie Casemore offers the following tips:
- Avoid reducing pumping sessions before baby is two to three months old unless you are getting over 1100ml (40oz) per day
- Continue night pumping until baby is at least three months old
- Drop pumping sessions slowly e.g. only one per month to make sure your overall milk volume is not affected
- Alternatively, try gradually spacing the time between pumps e.g. instead of pumping every two or three hours try every three or four hours. Aim to still pump the same total of minutes a day.
- Express enough milk to stay comfortable if you feel uncomfortably engorged at any time.
How do I stop exclusively pumping?
As with stoping breastfeeding this is best done slowly to give your breasts time to adjust and avoid getting blocked ducts or mastitis. Over a period of a few weeks to a month or so try gradually shortening each pumping session by a few minutes. Look out for any engorgement and express enough milk to stay comfortable if you do feel painfully engorged.
Summary
Exclusively pumping breast milk to feed a baby is a viable alternative to breastfeeding for some women. It is important to find both the right pump and the right pumping schedule for any individual mother to maximise her milk supply.

