Breast surgery may be carried out to alter the appearance of breasts (cosmetic surgery) or for medical or health reasons. Surgery that changes the appearance of the breasts includes breast augmentation (breast implants), breast reduction surgery or nipple surgery. Medical reasons for breast surgery might include taking a sample of a suspicious lump for analysis (a biopsy), or surgical drainage of a breast abscess. Any type of breast surgery could cause challenges for breastfeeding. This article looks at how breast milk is made, how surgical procedures can affect breastfeeding and how to get breastfeeding off to a good start following breast surgery.
How breast milk is made and released
Breast milk is made in the breast and released (“let-down”) to the baby or pump thanks to specific nerves and hormones (chemical messengers).
Where milk is made
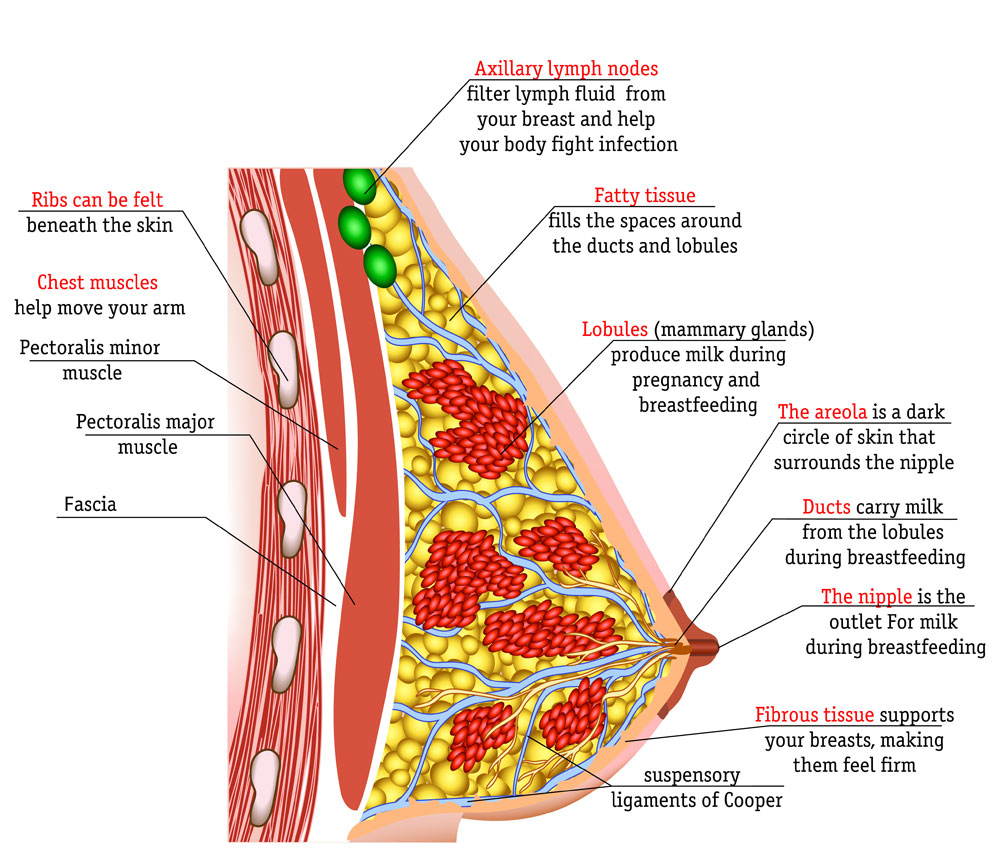
Inside the breast are lots of milk producing sacs (alveoli) that are arranged in clusters (lobules/lobes) and connected to the nipple by a network of fine tubes (ducts) through which the milk travels. The alveoli and ducts are interspersed and inter-connected with fatty tissue, blood vessels, nerves, lymphatic system (a drainage system for waste products) and supporting connective tissue. Two thirds of the milk making tissue (also known as glandular tissue) is said to be within 30 mm of the base of the nipple.12 Any damage to the milk making tissue could affect future milk production.
How milk is released to the nipple
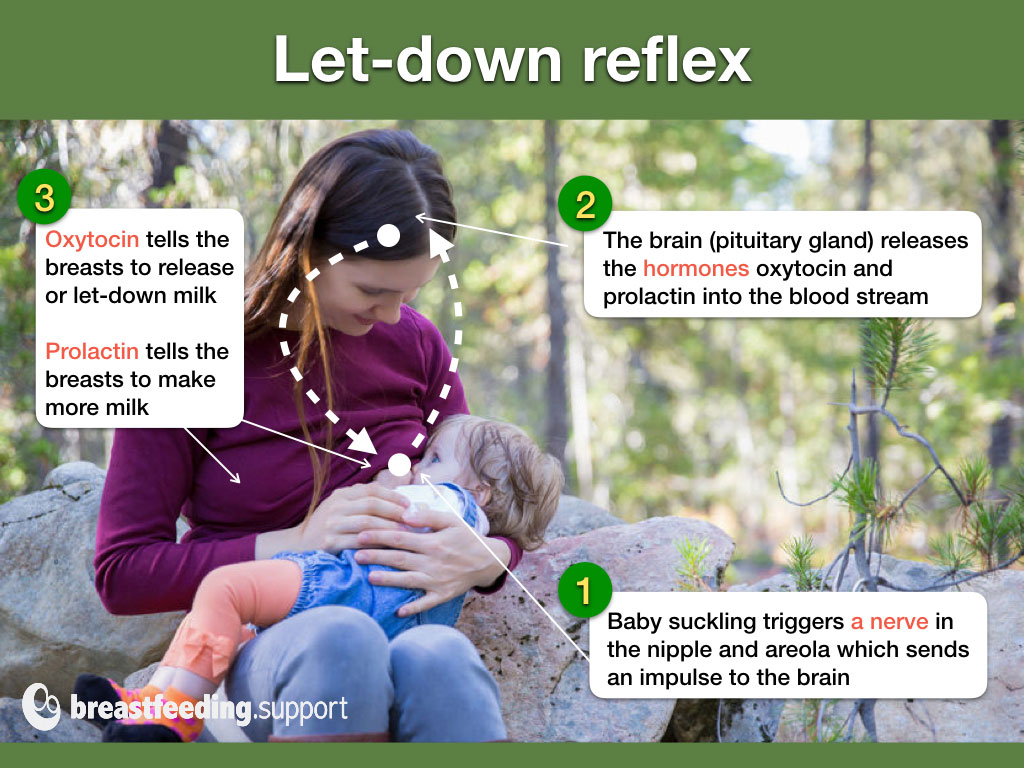
When a baby suckles (or a mother pumps or hand expresses) this triggers the milk ejection reflex or let-down reflex. A nerve in the sensitive areola and nipple (called the fourth intercostal nerve) is triggered by the baby’s suck—or hand/pump. The nerve carries a signal to the pituitary gland in the brain to release the hormones oxytocin and prolactin. Oxytocin releases breast milk from the milk making cells into the ducts and the milk then flows towards the nipple. Prolactin instructs the breast to make more milk. Any damage to the nerve that stimulates the pituitary gland could affect let-down and milk production.
How breast surgery affects breastfeeding
Whether breastfeeding is negatively affected after any type of breast surgery will depend on:
- Functioning glandular tissue. The amount of milk making tissue (alveoli and ducts) that has been damaged or removed during surgery may mean a full milk supply may not be possible.
- Nerve damage. If the nerve supply to the nipple or breast has been damaged or severed this can affect milk production and/or let-down. Although it is possible to condition the let-down to other triggers, see Let-Down Reflex: Too Slow? by Kelly Bonyata.
- Complications. Any post surgery complications such as infections, reconstruction surgeries, necrosis (tissue death due to loss of blood supply), or hematoma (a pocket of blood under the skin) can cause further challenges for breastfeeding.
- Pain and sensitivity. Some mothers find their breasts are very painful and much more sensitive after breast surgery which can make breastfeeding difficult. Nipple vasospasm can be more common after breast or nipple surgery (see below). Conversely, some mothers may lose sensation in the nipple due to damaged nerves—affecting the let-down reflex and the ability to feel the baby’s attachment (latch).
- Scar tissue and engorgement. Scar tissue can cause pain and firmness in the breast. Thick scar tissue can extend into milk ducts and affect the milk supply. The scar pattern on the surface of the breast doesn’t reveal the extent of scar damage that may be deeper in the breast. If areas of the breast are unable to drain freely, there may be excessive engorgement or blocked ducts which could lead to mastitis.
- Time since surgery. Damaged nerves and ducts can reconnect over time. And each breastfeeding experience since the surgery will provide an opportunity for more healing and growth of glandular tissue.
- Breastfeeding management. There may be other factors affecting breastfeeding apart from surgery including whether breastfeeding got off to a good start.
- Determination. Personal attitude and determination to breastfeed can be helpful to get breastfeeding established.
Specific challenges relating to individual surgeries or procedures will be discussed below.
#1 Breast augmentation
Breast augmentation involves making breast size bigger, usually by inserting a man-made breast shape or “breast implant” under the skin. Breast implants are made of a synthetic substance called silicone and are filled with either silicone gel or salt water (saline).
Can you breastfeed with breast implants?
Some mothers can breastfeed and make a full supply of milk with breast implants without any particular difficulties but others are not as successful. Reports vary between 30% to 80% of mothers with implants achieving a full milk supply.34 More independent research without bias to the cosmetic surgery industry is needed.
Challenges affecting breastfeeding
For a full description of the breastfeeding challenges associated with breast augmentation see Breastfeeding With Implants. Considerations include:
Milk making tissue present before surgery
A mother may have decided to have breast implants because her breasts had never really developed and she had very little breast tissue to begin with. There are several underlying medical issues that can have a bearing on glandular tissue.
The position and size of the implant
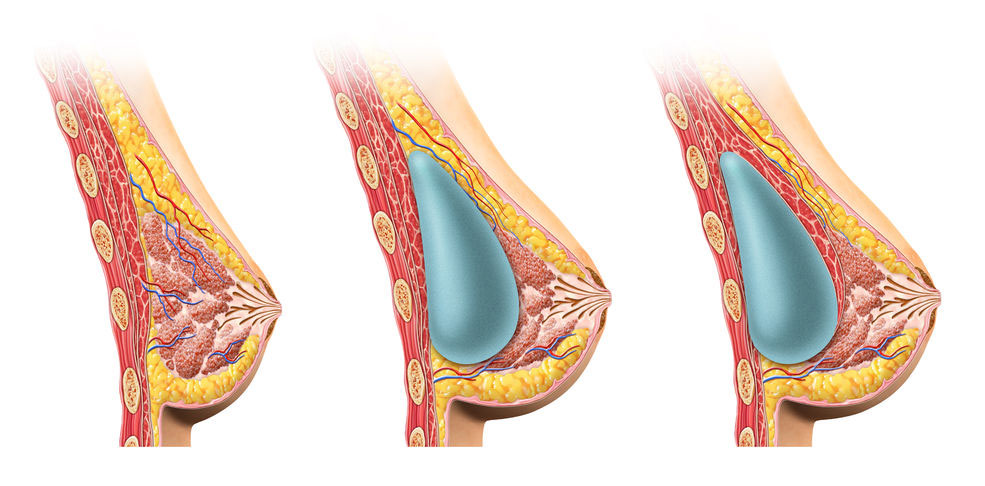
Whenever breasts are very full or engorged, milk production slows down. A breast implant has the potential to exert pressure on the breast tissue and mimic engorgement—slowing or limiting milk production. The larger the implant the greater the potential effect. There may be less pressure on the milk making tissue when the implant is placed beneath the muscle layer5 (see picture) but more research is needed.
Surgical technique
How the implant is inserted will affect how much glandular tissue or how many milk ducts, nerves or blood vessels are damaged during surgery. Surgical techniques include:
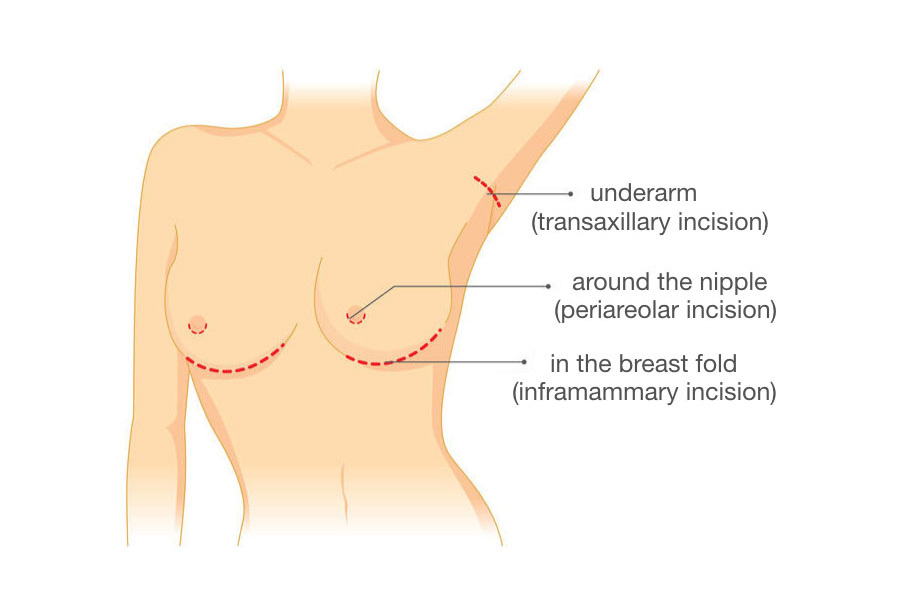
- Under the breast (inframammary)—an incision is made under the breast where the breast meets the chest wall. This type of surgery has less potential to cause issues for breastfeeding.
- Around the areola (periareolar)—an incision is made around the edge of the areola. This reduces visible scarring on the breast surface but is more likely to cut important nerves and ducts.
- Via the armpit (axillary enlargement)—the breast implant is inserted via an incision by the armpit to avoid scarring. Saline implants tend to be more common with this technique, placed under the gland or muscle.6
Complications
Breast implants are not life time devices and will need replacing at some point due to breast changes, rupture/leaking of the implant or other complications.7 Complications can include hardening of the breast around the implant (capsular contracture), long-term pain, heightened or reduced sensitivity to touch, pressure in the breast, scar tissue or further surgery to change the type, size or position of the implant.[/ref]8 Follow up surgery can cause further damage to breast tissue.
Safety issues controversy
General health concerns include an increased risk of a specific type of immune system cancer (anaplastic large cell lymphoma), breast implant illness, inflammation and autoimmune symptoms.9 Whether a pregnancy with breast implants or breastfeeding with implants in place is safe for the developing baby is unclear; there seem to be different opinions and a gap in research.
#2 Breast reduction
In breast reduction surgery an amount of breast tissue is surgically removed to reduce the size of the breast, this could be for medical or cosmetic reasons or both.
Can you breastfeed after a breast reduction?
Some mothers can breastfeed and make a full or partial supply of milk, others are not as successful. Exactly how breast reduction surgery can affect breastfeeding will depend on the type of surgery and time since surgery as well as the general considerations above such as how much breast tissue remains, whether important nerves and ducts have been damaged or whether there were complications.
Challenges affecting breastfeeding
For a full description of the breastfeeding challenges associated with breast reduction see Breast Reduction and Breastfeeding. Considerations include:
Surgical technique
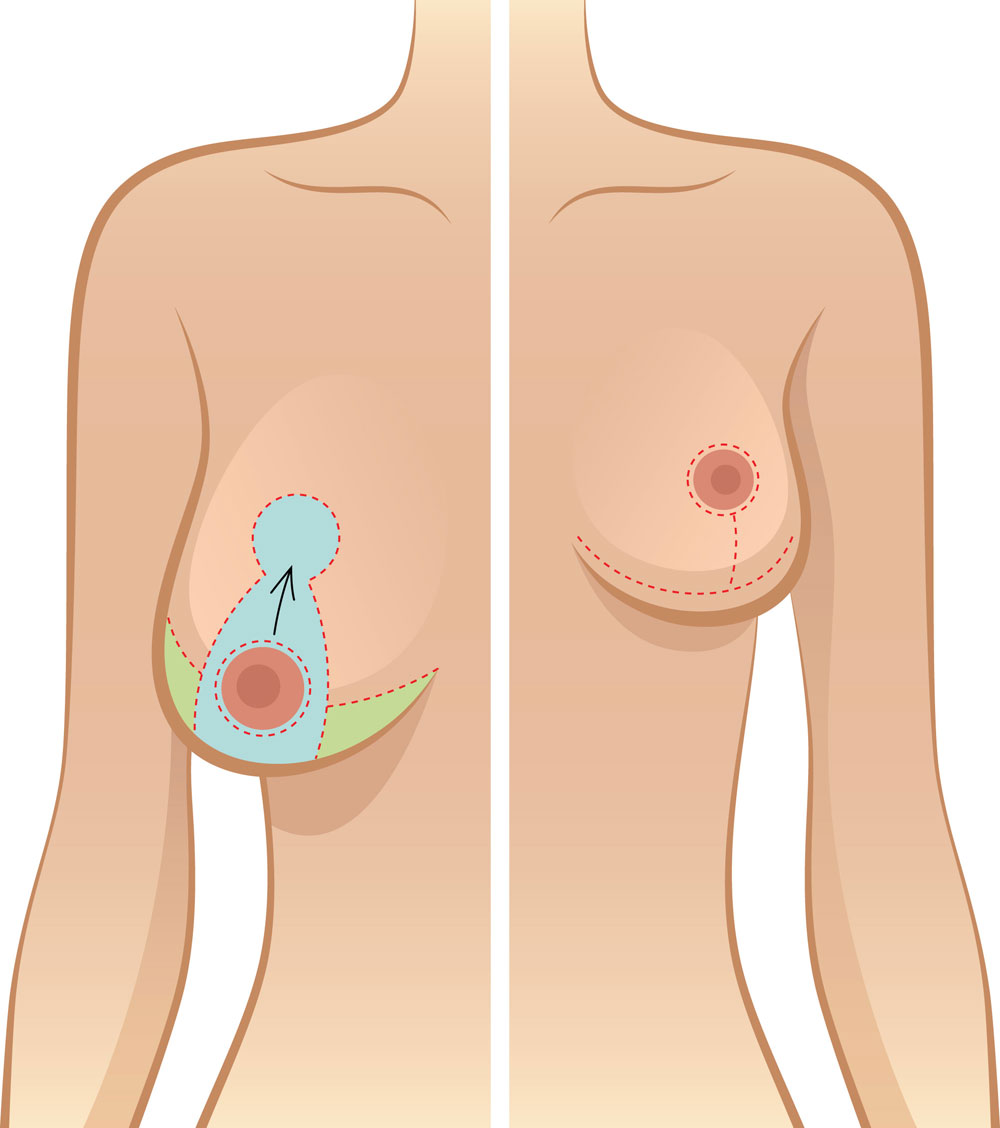
Where the incisions are made, whether important nerves, ducts and blood vessels have been cut or damaged, and whether the nipple has been repositioned will all affect breastfeeding. Techniques used to reduce breast size are described below:
- Fat removal (liposuction)—a suction tube is inserted into the breast to remove fat deposits
- Anchor type or inverted-T (inferior pedicle technique)—a cut is made around the nipple with an anchor shaped incision below the nipple. The nipple is repositioned on a stalk of breast tissue (pedicle) that is still attached to its nerves, ducts and blood supply. This type of scar pattern may also be seen with a breast lift procedure (mastopexy) where breasts are reshaped by the cosmetic surgeon.
- Periareolar breast reduction technique—an incision is made around the areola and excess breast tissue is pulled out from under the nipple. Glandular tissue and nerves may be damaged with this approach.
- Free nipple graft—involves completely removing the nipple and grafting it back to a new position on the reshaped breast. As the nerves, milk ducts and blood vessels are severed this causes significant damage. Successful breastfeeding is unlikely although it is possible for some nerves and ducts to reconnect over time and some sensitivity in the nipple may return.
Time since surgery
Removing sections of the breast will damage milk making tissue, ducts and nerves. However there is potential for some recovery over time;
- Healing of nerves. Nerves have potential to repair. A website dedicated to breastfeeding after breast surgery states it can take nerves five years to recover significantly.10
- Repair of ducts and glandular tissue. Hormones associated with menstruation, pregnancy and breastfeeding provide more opportunity for growth and repair of ducts and glandular tissue.
Nipple vasospasm
A nipple vasospasm is when the blood vessels in the nipple narrow or contract, squeezing the blood from the nipple so that nipples may temporarily look white just after a feed. Nipple vasospasm can be very painful. Mothers who have had breast or nipple surgery seem to be at greater risk of getting nipple vasospasm when they are breastfeeding.11 As nipple vasospasm can have other causes apart from breast surgery it’s important to check baby’s latch and positioning with a breastfeeding specialist and see Nipple Vasospasm and Breastfeeding for more information.
#3 A biopsy/draining an abscess
Any surgical procedure on a breast has the potential to affect breastfeeding including a biopsy or abscess:
- A breast biopsy. A biopsy is a medical test to take a sample of a lump or suspicious mass for further examination. A biopsy may involve surgery (cutting into the breast to remove a sample of tissue) although core needle biopsy (taking a sample with a needle guided by ultrasound) is the preferred diagnostic procedure as it is less invasive.
- A breast abscess. A breast abscess is a pocket of pus deep within the breast. Over a certain size a breast abscess requires draining to release the infection (pus). Incision and drainage involves cutting into the breast to release the infection and inserting a breast drain to allow the pus to drain away and the wound to slowly heal from the inside.
Challenges affecting breastfeeding
Breastfeeding challenges include the possibility of scar tissue, nerve damage, damage to milk making tissue or complications. A fistula can be a complication arising from a biopsy, abscess or surgical procedure on a lactating breast.1213 A fistula is when breast milk constantly leaks from the skin of the breast from a damaged milk duct below it. See Medical Tests While Breastfeeding and Do I Have a Breast Abscess? for more information.
#4 Nipple surgery and nipple piercings
Surgery to nipples may include reducing nipples in size, reducing the size of the areolae (the darker coloured skin around the nipples), enlarging nipples, or releasing inverted nipples (when nipples are pulling into the breast instead of pointing outwards). Nipple piercing is a procedure to the nipple that makes permanent holes through the nipple to insert jewellery. How any nipple procedures could affect breastfeeding will depend on the type of procedure and the extent of any scar tissue.
Can you breastfeed after nipple surgery or piercings?
There are several openings at the surface of each nipple (nipple pores) through which milk is released. Research has found an average of around nine nipple pores per nipple.14 It follows that if a mother doesn’t have many nipple openings to begin with, a procedure that damages several nipple pores could affect breastfeeding.
Challenges affecting breastfeeding
For a full description of the breastfeeding challenges associated with breastfeeding with pierced nipples see Breastfeeding With Pierced Nipples. General considerations after nipple procedures include:
- Blocked nipple pores. If blocked or scarred nipple pores prevent an area of the breast from draining this may cause blocked ducts or mastitis
- Fast flow or slow flow. Damaged nipple pores may stop milk flowing freely or conversely, milk may pour out quickly from the piercing hole in the case of pierced nipples.
- Low milk supply, low weight gain. If the breasts are not being thoroughly drained this will ultimately limit milk production and a baby’s weight gain.
- Increased risk of infections. There is a higher risk of bacterial infections and infective mastitis with pierced nipples.
- Reduced sensitivity or increased sensitivity. Some mothers find their nipples can change in sensitivity following nipple surgery. Losing sensitivity could affect let-down and hypersensitivity could mean breastfeeding is very painful.15
Maximising milk supply
In view of the potential challenges that could limit a mother’s milk supply after breast surgery, it is important to maximise the available milk by getting breastfeeding off to a good start whenever possible. If can be helpful to see a breastfeeding specialist such as an International Board Certified Lactation Consultant (IBCLC) for an antenatal breastfeeding appointment and meet with other breastfeeding mothers for support and information. Suggestions include:
Antenatal expression of colostrum
Parents who are not at high risk for premature birth, could discuss the latest research on antenatal expression of colostrum (the first breast milk present before birth) with their health professionals.16 Antenatal expression is sometimes mentioned as a way to help establish a full milk supply more quickly. If colostrum is harvested and stored (frozen), this can reduce the need for early formula supplements in the event of any breastfeeding challenges. Even if colostrum isn’t collected antenatally, getting familiar with hand expressing techniques can be useful postnatally to relieve any breast engorgement or to provide a supplement if baby struggles to latch at first. Check Expressing Colostrum Antenatally for advantages, disadvantages and precautions.

A natural birth
Where possible, an active, natural birth can help to support breastfeeding by minimising birth medications and interventions. Pain killers and epidural drugs can make a baby sleepy and uninterested in breastfeeding for several days and intravenous fluids can cause extra fluids to enter breast tissue making latching more difficult and limiting milk flow. See No Breast Milk After Delivery for more information about how birth practices affect breastfeeding.
Breastfeed in the first hour after birth
Babies have strong feeding instincts in the first hour after birth, birth hormones help maximise milk flow and early feeds send an important signal to the breast to start milk production.17
If a baby is unable to breastfeed
Until a baby can breastfeed, hand expressing will send the message to the milk factory that milk production is needed, and provide a supplement to keep baby well fed. It’s important to express milk as often as a baby would breastfeed; at least every two hours to keep milk flowing. See When Baby Won’t Breastfeed for more reading.
Frequent feeds
Frequent breastfeeding or expressing breast milk at least every two to three hours in the early weeks helps milk production because the number of feeds requested now helps predict the level of milk production needed going forward.
Skin-to-skin contact
Skin-to-skin contact lets a baby use his senses of touch, smell, sight and taste to help him find the nipple and breastfeed. Skin-to-skin contact promotes the hormones needed for milk production, and regulates a baby’s heartbeat, temperature and breathing. See Why Skin-to-Skin? for more benefits of skin-to-skin contact and see Scratch Mittens and Breastfeeding.
Comfortable latch
Ensure baby has a big mouthful of breast tissue as well as a nipple in their mouth (deep latch) and comfortable positioning. A deep latch helps to drain the breasts thoroughly and promote milk production. See Latching Tips and Breastfeeding Positions for Newborns.
Galactagogues
A galactagogue is a food, herb or drug that might help to increase milk supply. Not everyone agrees whether these are helpful but some herbs are reputed to be useful for building breast tissue or assisting with the let-down reflex. For more information see What is a Galactagogue?
Know when help is needed
There are several ways to tell if a baby is getting enough milk and a number of red flags to look out for that indicate that breastfeeding may not be going as well as it could. If any of the following problems occur, contact a breastfeeding specialist to help you:
- Pain. Sore nipples are generally a sign that baby isn’t attached to the breast as well as they could be and, if this is the case, it could interfere with milk production. However there can be many Causes of Sore Nipples. Breast surgery itself could be a cause of very painful nipples, nipple vasospasm, or pain in the breasts and in some cases may cause reduced nipple sensation.
- Not many dirty nappies. When milk goes into your baby, poop will come out! Breastfed Baby Poop describes the colours and amount of poop that usually indicate feeding is going well and see Is My Baby Getting Enough Milk?
- Jaundice. Jaundice (yellowing of the skin after birth) can be prolonged if a baby isn’t feeding well, see Jaundice in Breastfeeding Babies.
- Prolonged engorgement. Excess engorgement is a risk factor for reducing a milk supply. After breast surgery there is more chance of severed ducts or scar tissue interfering with breast drainage leading to severe engorgement. In some cases after surgery, there may not be any engorgement and milk may not seem to “come in”. If any areas of the breast don’t have an outlet to the nipple and are not relieved by gentle massage, or hand expressing, milk production will eventually be shut down in those areas. See Engorged Breasts and Engorgement Relief When Milk Won’t Flow.
- Baby not gaining weight. Although some weight loss is normal in the first week, after this time weight gain is a useful indicator that all is well with breastfeeding. If baby is not gaining 1oz or 30-40g per day, or is still losing weight, seek good breastfeeding help and see Baby Not Gaining Weight. Parents will need to be aware that some mothers who have had breast surgery will not be able to produce a full milk supply despite maximising their milk supply and supplements may be needed. Bear in mind there can be other causes of low milk supply aside from breast surgery and it can be helpful to see an IBCLC for an assessment.
If supplements are needed
If supplements are needed these can be given by bottle in a breastfeeding friendly way or at the breast using a supplemental nursing system. Providing some or all supplements at the breast can give a mother and baby the experience of breastfeeding.
Summary
Any surgery to the breast has the potential to damage milk-making tissue or the nerves that are needed for lactation and this may affect milk supply. Breast surgery can lead to further complications such as ongoing pain, infection, scar tissue, engorgement or the need for further corrective surgery. In order to maximise a mother’s milk supply it is helpful to get breastfeeding off to the best start possible. If problems arise, the sooner they can be resolved the better. Signs that breastfeeding might not be going well include breastfeeding pain (sore nipples), baby not pooping, prolonged jaundice, prolonged engorgement and a baby who isn’t gaining weight. It can be useful to have a consultation with a breastfeeding specialist so that other possible reasons for low milk supply can be ruled out from the medical history and the milk supply can be maximised with a tailored plan. Some mothers may not be able to make a full supply of breast milk after some procedures.

